Services
-
PET-CT

 PET / CT (abbreviation for Positron Emission Tomography-Computed Tomography) is currently the most advanced imaging technique in cancer and dementia diagnostics. The combination of PET and CT in one device allows the detection of tumours, inflammations or neurological disorders earlier and more accurately than it was possible with previous methods.
PET / CT (abbreviation for Positron Emission Tomography-Computed Tomography) is currently the most advanced imaging technique in cancer and dementia diagnostics. The combination of PET and CT in one device allows the detection of tumours, inflammations or neurological disorders earlier and more accurately than it was possible with previous methods.In PET scanning, patients receive a small amount of a radioactive substance, usually fluorodeoxyglucose (FDG), which is a slightly altered glucose molecule. This substance accumulates in the organism in regions of intense metabolic activity. The increased glucose consumption by tumour compared to normal cells, is lead to an increased uptake of FDG. The pathological cells are then visible as bright dots on the PET images.
At the same time, the computed tomography shows a 3 dimensional reconstruction of the anatomy of the body.
Afterwards the PET and CT images are merged together in the device. This enables the examiner to discover even the smallest tumours very early. It can also be determined whether the tumours are benign or malignant.
The early diagnosis allows the treating physician to choose the best treatment for the patient: whether surgery, chemotherapy, radiation or a combination of different treatment options. A PET/CT follow-up scan can show whether/if the patient responds to treatment.
Moreover, the PET/CT scan is currently the most sensitive method to detect numerous brain diseases. It is possible to detect dementia before other methods show abnormalities. Early diagnosis is important in the case of Alzheimer’s disease, because only timely treatment can slow down the progression of the disease. The device is also able to recognize other brain disorders such as Parkinson, even if the patient has very few symptoms.

Picture: PET/CT of an esophageal carcinoma (esophageal cancer): the CT scan is presented on the left, the PET-image is shown on the right. The merged PT/CT image is located in the middle. The bright dot to the left is the original tumour, the smaller dot to the right a metastasis in a lymph node.
The PET/CT method is mainly used for diagnosing the following types of tumours:
– lung cancer (bronchial carcinoma), pulmonary nodule
– colorectal cancer (colorectal carcinoma)
– breast cancer
– prostate cancer (carcinoma of the prostate)
– black skin cancer (malignant melanoma)
– malignant lymphoma (Hodgkin’s disease and non-Hodgkin’s lymphoma)
– esophageal cancer (carcinoma of esophagus)
– thyroid (carcinoma of the thyroid gland)
– pancreatic cancer (
– neuroendocrine tumours (e.g. carcinoid)
– ovarian cancer (ovarian carcinoma)
– head and neck cancer
– bone and soft tissue tumours
– testicular cancer
– cerebral tumours
– examination of metastases when primary tumour is unknown (CUP syndrome)The PET/CT method is also used for:
– search for an inflammatory focus (fever of unknown origin)
– early detection of dementias such as Alzheimer’s disease
– distinction of different forms of dementia
– diagnosis of movement disorders
– epilepsy-
Radioiodine therapy
Radioiodine therapy is a nuclear medicine procedure to treat different kinds of thyroid diseases. It is considered a [non-invasive] gentle alternative to surgery. Radioiodine therapy is used in different types of thyroid hyperfunction (hyperthyroidism), e.g. Basedow’s disease), autonomic dysfunction of the thyroid gland (e.g. autonomous adenoma) or certain kinds of thyroid cancer (papillary or follicular carcinoma). An enlarged thyroid gland (goitre) can also be treated with this therapy.
In radioiodine therapy, radioactive iodine 131 is administered. The advantage is that the substance is absorbed only by the thyroid gland and only acts there.
If the thyroid gland had to be resected /removed surgically because of a carcinoma, it is common to perform a radioiodine therapy approximately three weeks later. This allows to remove remaining healthy thyroid tissue and the destruction of the remaining malignant tissue.
Examination and therapy
Based on the results of the preliminary examination (blood examination, ultrasound and scintigraphy of the thyroid gland) it is decided whether radioiodine therapy is indicated.
If so, you will stay as inpatient at the DKD Helios Clinic. Radioactive iodine will be given to you in the form of one or more small capsules after a radio iodine test has been made in advance. The dose is calculated individually and the substance is well tolerated. Only a few patients noticed a slight sore throat, which disappears after a few days.
Over the next days the radioactivity of your thyroid gland will be measured. If it has decayed to a certain value, we can discharge, usually after three to seven days.
During your stay, you are not allowed to receive visits, due to radiation protection reasons. You are also not allowed to leave the station. However, you have regular contact with doctors, nurses and of course other patients. There is also a telephone, TV and internet connection (WLAN) at your disposal.Preparation before and after the examination
Some patients must take a thyroid hormone before therapy. You will be informed if you need to take the hormone when arranging the appointment.
Please avoid the intake of larger amounts of iodine before therapy (for example in contrast medium or in the medicine amiodarone).
Usually, the stay at the hospital is about three to seven days.
The therapeutic effect usually occurs only after a few weeks. Therefore, follow-up examinations are necessary after the radioiodine therapy. These examinations can be made at our practice or at your treating physicians’ practice.
Please do not hesitate to contact us, if you have any further questions!
-
Radioreceptor therapy (DOTATOC)
Lu-177-DOTATOC- or Y-90-DOTATOC-therapy
PRRT (peptide radio-receptor therapy) of somatostatin receptor-positive malignant tumours by using a peptide DOTATOC labelled with the radioactive beta emitter Yttrium-90 or Lutetium-177.
Prof. R. P. Baum performed most of the cancer therapies with Lu177-DOTATOC in neuroendocrine tumours across Germany.
1. Which tumours can be treated?
It is possible to treat tumours and metastases that have an increased somatostatin receptor occupancy on the surface of the cancer cell. This receptor occupation is detected by DOTATOC PET/CT, a necessary preliminary examination, which is performed previously in the practice. PET/CT allows to accurately determine the number of docking sites for subsequent therapy on tumour cells/metastases by using so-called uptake values (SUV) and thus to predict whether Lu177-DOTATOC or Y90-DOTATOC therapy would be useful and if the therapy can be successful: THERANOSTICS principle – irradiation is targeted to what is previously visible on PET/CT.
2. Mode of action of Lu-177/Y-90-DOTATOC therapy
PRRT is used for nuclear medicine treatment of somatostatin receptor-positive metastases or tumour recurrences, which no longer respond to other treatments. For this purpose, a molecule labelled with the beta emitter Lu-177 or Y-90 is used. The range of the beta emitter Lutetium-177, for example, is about 2 mm in tissue. Very large tumours can also be treated, since the molecule penetrates almost any tumour depth. Due to the short range, healthy tissue can be spared as far as possible. The molecule labelled with the beta emitter is applied into a vein of the arm and accumulates very quickly in the metastases or tumour recurrences which have been previously detected by DOTATOC PET/CT, as well as it accumulates in the primary tumour – what is previously visible in PET/CT is also irradiated – “we see what we treat”. The therapy effect thus depends on the storage intensity in the PET/CT. The therapy emitter destroys the DNA of the tumour cells, which should slow down the growth of the tumour or cause it to regress.
3. Course of therapy
The duration of inpatient admission to DKD Helios Hospital is approximately 3-4 days. Unfortunately, you are not allowed to receive visitors or leave the ward during your inpatient stay, for reasons of radiation protection. However, you will have regular contact with doctors, nursing staff and, of course, your fellow patients. You will also have access to telephone, television, and Internet connection (WLAN).
In advance to the therapy, necessary examinations (laboratory control, whole-body DOTATOC-PET/CT, possibly kidney- or salivary gland scintigraphy, sonography) are performed. The results of the examination are discussed in detail before the treatment.
It is necessary to drink at least 1.5 litres of liquid, on the therapy day, to keep radiation exposure as low as possible (accelerated excretion).
The therapy substance is administered intravenously via an arm vein what takes only a few minutes. The excess therapy substance not docked to the metastases/tumours is predominantly excreted renally. Infusion therapy (parenteral fluid administration) is given to reduce renal burden. It is extremely rare that patients experienced nausea after therapy.
After injection of the therapy substance, the patient must remain on the therapy ward for at least 48 hours (this is a legal requirement, that cannot be negotiated).
The control of the accumulation intensity in the metastases as well as measurements of the degradation of the therapy substance in the rest of the body are carried out in the nuclear medicine practice as scintigraphic whole-body images as well as with SPECT/CT (tomography/slice examination) of the tumour regions.
The therapy is usually repeated several times at intervals of 3-4 months. Before a new therapy course, a DOTATOC-PET/CT is usually performed to monitor the success.
4. Potential side effects
The number of red blood cells (erythrocytes), platelets (thrombocytes) and white blood cells (leukocytes) may decrease. Therefore, the blood count must be checked at certain intervals after therapy. Even after repeated therapy, there is usually no restriction of renal function, renal function is monitored. Due to accumulation in the lacrimal and salivary glands, radiogenic sialadenitis (dry mouth) may occur (this has been observed rarely). Allergic reactions may (theoretically) occur during administration (never observed to date). Long-term side effects or harmful long-term effects have not occurred/are not known so far.
5. The therapy cannot be used in the following diseases:
– Acute infections with fever
– Severe bone marrow insufficiency
– High-grade renal insufficiency
– Myocardial infarction within the last 6 weeks
– Rapidly progressive second malignanciesContact: Prof. Dr. med. Richard P. Baum, CURANOSTICUM Wiesbaden-Frankfurt
Email: baum@curanosticum.de-
Radio-ligand-therapy (PSMA)
Lu177-PSMA therapy
RLT (radio-ligand therapy) of therapy-refractory (prostate carcinoma no longer responds to hormone therapy), metastasised prostate carcinomas with lutetium-177 PSMA.
Prof. R.P. Baum performed the world’s first therapy with Lu177-PSMA for prostate cancer and has successfully treated thousands of patients with this method. Since Prof. R. P. Baum joined us, we also offer cancer therapies with Lu177-DOTATOC for neuroendocrine tumors.
1. Which tumors can be treated?
All metastases can be treated that have PSMA (prostate specific membrane antigen) on the surface of the cancer cell. This is determined by PSMA PET/CT (positron emission tomography), a necessary preliminary examination which is carried out in our practice in previously. PET/CT makes it possible to precisely determine the number of docking sites for the subsequent therapy on the tumor cells/metastases based on so-called uptake values (SUV) and thus to predict whether Lu177 therapy makes sense at all and with what probability success can be achieved: THERANOSTICS principle – irradiation is targeted to what is previously visible in PET/CT.
2. Mode of action of lutetium-177 PSMA therapy
Radio-ligand therapy (RLT) is used for the nuclear medical treatment of PSMA-positive, mostly hormone-resistant metastases or tumor recurrences that no longer respond to other treatment methods (hormone therapy, percutaneous radiotherapy or chemotherapy). A molecule labelled with the beta emitter Lu-177 (ligand, PSMA inhibitor) is used for this purpose. The range of the beta emitter lutetium-177 in the tissue is approx. 2 mm, but also very large tumors can be treated, as the molecule penetrates into practically every tumor depth. Healthy tissue is spared as far as possible.
The molecule labelled with the beta emitter is applied into a vein in the arm and accumulates very quickly in the metastases or tumor recurrences previously detected by the PSMA PET/CT or also in the primary tumor – what is previously visible in the PET/CT is also irradiated – as you say in English “we see what we treat”. The therapy effect thus depends on the storage intensity in the PET/CT. The therapy emitter destroys the DNA of the tumor cells, which causes the tumor findings to regress (in approx. 70 %) or at least to slow down their growth (in approx. 15 %). In a few cases, the tumour cells are destroyed.
3. Course of therapy
The duration of inpatient admission to the DKD is 2 to 3 days. During your inpatient stay, you are unfortunately not allowed to receive visitors or leave the ward for radiation protection reasons. However, you will have regular contact with doctors, nursing staff and, of course, your fellow patients. You will also have access to telephone, television, and internet connection (WLAN).
Before the therapy is carried out, the necessary examinations are made (laboratory control including PSA determination, whole-body PSMA PET/CT, possibly kidney or salivary gland scintigraphy, sonography, urological presentation). The examination results are discussed in detail before treatment.
On the day of therapy, at least 1.5 litres of fluid must be drunk to keep the radiation exposure as low as possible (accelerated excretion). The therapy substance lutetium-177 PSMA is administered intravenously via a vein in the arm and only takes a few minutes. The excess therapy substance which did not dock to the metastases/tumors is predominantly excreted renally. Infusion therapy (parenteral fluid administration) is given to reduce renal stress. Nausea occurred extremely rarely after therapy.
After injection of the therapy substance, the patient must remain on the therapy ward for 48 hours (this is a legal requirement that cannot be negotiated).
The control of the accumulation intensity in the metastases as well as measurements of the degradation of the therapy substance in the rest of the body are carried out in the practice for nuclear medicine as scintigraphic whole-body images as well as by a SPECT/CT (tomography/slice examination) of the tumor regions.
The therapy is usually repeated after 8 to 12 weeks. Before a new course of therapy, a PSMA-PET/CT may be performed to monitor the success.

4. Potential side effects
The number of red blood cells (erythrocytes), blood platelets (thrombocytes) and white blood cells (leucocytes) may decrease. Therefore, the blood count must be checked at certain intervals after the therapy. Even after repeated therapy, there is usually no restriction of kidney function; renal function is monitored. Due to accumulation in the lacrimal and salivary glands, radiogenic sialadenitis (dry mouth) may occur (this has been observed only rarely). Allergic reactions may (theoretically) occur during administration (never observed so far). Long-term side effects or harmful long-term effects have not occurred/are not known so far.
5. The therapy cannot be used for the following diseases:
– Acute infections with fever
– Severe bone marrow insufficiency
– Severe renal insufficiency
– Heart attack within the last 6 weeks
– Rapidly progressive secondary malignanciesContact: Prof. Dr. med. Richard P. Baum, CURANOSTICUM Wiesbaden-Frankfurt
E-mail: baum@curanosticum.dePublications (Sample)
Baum RP, Kulkarni HR, Volkmer B, Bohuslavizki KH, Schuchardt C, Klette I, Singh A, Wester HJ
Theranostik des metastasierten Prostatakarzinoms mittels Lu-177 PSMA-Liganden in Kombination mit Ga-68 PSMA PET/CT
Nuklearmediziner 2015; 38:145-152Baum RP, Kulkarni HR, Schuchardt C, Singh A, Wirtz M, Wiessalla S, Schottelius M, Mueller D,Klette I, Wester HJ
177Lu-Labeled Prostate-Specific Membrane Antigen Radioligand Therapy of Metastatic Castration-Resistant Prostate Cancer: Safety and Efficacy
J Nucl Med. 2016l;57:1006-13Kulkarni HR, Singh A, Schuchardt C, Niepsch K, Sayeg M, Leshch Y, Wester HJ, Baum RP
PSMA-Based Radioligand Therapy for Metastatic Castration-Resistant Prostate Cancer: The Bad Berka Experience Since 2013
J Nucl Med. 2016;57(Suppl 3):97S-104SKulkarni HR, Singh A, Langbein T, Schuchardt C, Mueller D, Zhang J, Lehmann C, Baum RP
Theranostics of prostate cancer: from molecular imaging to precision molecular radiotherapy targeting the prostate specific membrane antigen
Br J Radiol. 2018; 91(1091):20180308Rahbar K, Ahmadzadehfar H, Kratochwil C, Haberkorn U, Schäfers M, Essler M, Baum RP, Kulkarni HR, Schmidt M, Drzezga A, Bartenstein P, Pfestroff A, Luster M, Lützen U, Marx M, Prasad V, Brenner W, Heinzel A, Mottaghy FM, Ruf J, Meyer PT, Heuschkel M, Eveslage M, Bögemann M, Fendler WP, Krause BJ
German Multicenter Study Investigating 177Lu-PSMA-617 Radioligand Therapy in Advanced Prostate Cancer Patients
J Nucl Med. 2017;58:85-90Fendler WP, Kratochwil C, Ahmadzadehfar H, Rahbar K, Baum RP, Schmidt M, Pfestroff A, Lützen U, Prasad V, Heinzel A, Heuschkel M, Ruf J, Bartenstein P, Krause BJ
Therapie mit 177Lu-PSMA-617, Dosimetrie und Nachsorge beim metastasierten kastrationsresistenten Prostatakarzinom
Nuklearmedizin. 2016 Jun 28;55:123-8-
Thyroid diagnostics and therapy
The thyroid gland is a butterfly-shaped organ that is in the front neck region. It produces the vital thyroid hormones. The most frequent thyroid disease in Germany is the “goitre”, an enlargement and / or nodulous change of the thyroid gland. This is usually caused by iodine deficiency. Besides, there are often immune diseases of the thyroid gland and less frequent thyroid cancer. If the level of the thyroid hormones is too high or low it might cause functional disorders in different organs. An overactive thyroid (hyperthyroidism) can manifest itself in nervousness, sleep disturbances, sweating, heart palpitations or weight loss. An underactive thyroid (Hypothyroidism) may be e.g. being cold or fatigue.
The size of the thyroid gland as well as different disorders of the thyroid gland can be detected with thyroid gland ultrasound. The disorders include thyroid nodules as well as inflammation or enlargement of the thyroid gland. An ultrasound may also be necessary for therapy monitoring and for tumour search. As a special method, we offer the ultrasound elastography of nodes, which can be used to examine how hard or soft a node is. This can help in assessing the benignancy or malignancy of a node.

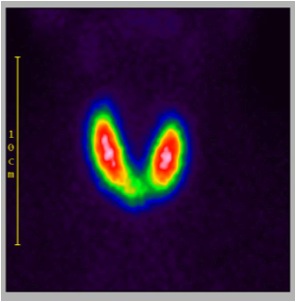
Figure: Thyroid scintigraphy displays the butterfly shape of the thyroid gland
Thyroid scintigraphy is a nuclear medical examination in which the function of thyroid nodules and the entire thyroid gland can be visualized. For this purpose, a small amount of a low-radioactive substance is administered to you. This substance will accumulate in the thyroid gland and emit rays. The rays can then be measured as an image (scintigram) with a gamma camera.
The examination makes it possible to assess the nodular changes of the thyroid gland and to determine whether normal, cold or hot nodes are present. “Hot” nodes work too much and can cause hyperthyroidism. “Cold” nodes work too little and can be malignant. Scintigraphy of the thyroid gland becomes necessary if nodular structures are detected in the thyroid gland or if we need additional information about thyroid’s function.
Examination procedure
To determine if your thyroid gland is infected, we first ask you about your complaints and your medication. We then examine you physically. In most cases, blood samples are taken, e.g. thyroid hormones and antibodies. The laboratory values indicate whether there is an over or under function of the thyroid gland. They can also indicate the cause of the functional disorder.
Thyroid ultrasound
The examination takes place in lying position. If it shows abnormalities, scintigraphy may be necessary to clarify the findings.
Scintigraphy of the thyroid
First, a small amount of a low-radiation marker substance will be injected. This substance will accumulate in the thyroid cells short time after the injection.
The substances used are very well tolerated; allergic reactions are not known. The radiation load is low and quickly degraded.
About fifteen minutes later images of the thyroid are recorded with a gamma camera. The recording takes about five to ten minutes.

Fig. 1: thyroid scintigraphy shows an over activity of the “hot” node in the thyroid gland (left), the healthy tissue is suppressed

Figure 2: the healthy tissue is active after a radioiodine therapy, the “hot” node is no longer active
Puncture of the thyroid gland
If a cold node – which might be malignant – is found it is often useful to take a tissue sample / biopsy. Cells are taken with a very fine needle (similar as when taking blood) and are examined microscopically.
Preparation before and after the examination
You may have your meals before the examination.
Please do not take your thyroid gland medication on the day of the examination.
Please inform us if you had had any tests or treatments using iodinated contrast material (for example X-ray/CT) or medication with high iodine load such as cordarex, as this might affect the accuracy of the scintigraphy.
We will send the examination results to your treating physician as soon as possible. He will then contact you to discuss the results as well as the possibility of a treatment.
Please do not hesitate to contact us if you have any further questions!
-
Myocardial scintigraphy

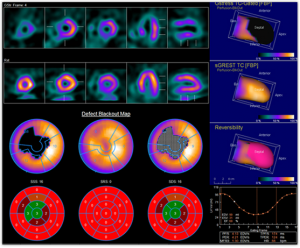
Figure: the blood flow of the heart is presented in different levels – above you can see the images under physical strain and below the stress and the rest images
Myocardial scintigraphy is a nuclear medical examination of the heart muscle. It allows to detect blood flow disturbances of the heart at an early stage.
The coronary vascular disease is the most common cause of such circulatory disorders. Plaques can narrow the coronary arteries and trigger a heart attack.
The myocardial scintigraphy is performed by applying a small amount of a low-radioactive marker substance. Depending on the blood flow, it accumulates in the heart muscle and emits radiation. The radiation can be measured as image (scintigram) with a gamma camera. The measurement is done under physical strain and at rest.
Examination procedure
Stress phase
First, you will be physically strained either on a bicycle ergometer or through medication.
Then, a small amount of a low-radiation marker substance will be injected. This substance will accumulate depending on the blood flow of the heart muscle. The substances used are very well tolerated; allergic reactions are not known. The radiation load is low and quickly degraded.
.
After the injection, you should have a rich breakfast and drink the sparkling water we provide. This is necessary to empty the gallbladder. With an empty gallbladder, the image quality will be decisively improved.After a short time of waiting (about twenty to thirty minutes), we will make so-called scintigrams, which means that a gamma camera will take pictures from the heart. This will only take a few minutes.
Rest phase
This time the examination is carried out without any previous physical exertion (for some patients this part of the examination is no longer necessary).
The two examinations usually take place the same day.
Preparation before and after the examination
Please do not take any heart or blood pressure medication or caffeine-carrying medication on the day of the examination and the evening before.
Caution: Some medication must be discontinued some time before the examination, but only after consultation with your doctor or cardiologist. These are especially some beta-blockers and nitro-glycerine. Please do not discontinue this medication without your doctor’s permission. If the examination at rest is carried out on another day, you can take your medication on this day as usual.
Please have only a small breakfast (half a roll, no banana, no chocolate).
Please DO NOT drink the following beverages in the morning: coffee, black or green tea, cola, cocoa (you should also not drink these beverages the day before).
Please bring a high-fat meal (e.g., rolls with cheese or cold cuts); After the injection, you can also have breakfast in the cafeteria of the DKD Helios Clinic.
Please wear comfortable clothes and shoes for cycling.
Please bring a towel with you.
We will send the examination results to your treating physician as soon as possible. He will then contact you to discuss the results as well as the possibility of a treatment.
Please do not hesitate to contact us if you have any further questions!
Download “Patient Information Myocardial Scintigraphy” (PDF)-
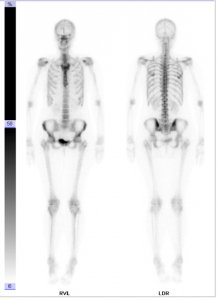
Bone scintigraphy
The skeletal or bone scintigraphy is a nuclear medical examination which can be used to detect pathological changes in the skeleton. For this purpose, a small amount of a low-radiation marker substance is administered. The substance accumulates in the bone structure and emits radiation. The radiation can be recorded as picture (scintigram) with a gamma camera.
It is possible to detect abnormal changes of the skeleton such as inflammation, bone fractures, signs of wear, bone tumours or bone metastases of a tumour at a very early stage due to this examination. It also detects loosening of joint prostheses.
Examination procedure
First, a small amount of a low-radiation marker substance will be injected. This substance will accumulate in areas where the metabolic level of the bones is elevated.
The substances used are very well tolerated; allergic reactions are not known. The radiation load is low and quickly degraded.
After that, first images of the skeleton are taken with a gamma camera for about twenty minutes.
Images of the skeleton will be taken once again about two to three hours later, as the metabolism of the bones is relatively slow.
The examination lasts approximately three to four hours, including waiting time. You do not have to stay at the practice while waiting. You may go home, to work or go at the cafeteria.
Preparation before and after the examination
You may have meals in advance to the examination, as well as take your medication as usual.
After the injection of the low-radiation marker substance, please drink at least half a litre of water.
Please empty your bladder shorty before the pictures are taken. Patients with urine bags should replace the bag with a new one.
We will send the examination results to your treating physician as soon as possible. He will then contact you to discuss the results as well as the possibility of a treatment.
Please do not hesitate to contact us if you have any further questions!
-
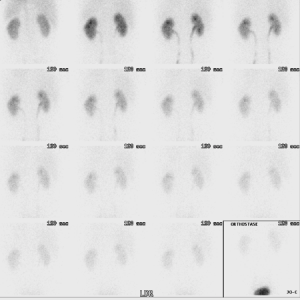
Pulmonary scintigraphy
A pulmonary scintigraphy is a nuclear medical examination with which the blood circulation and ventilation conditions of the lung can be detected. Thereto, a small amount of a low-radiation marker substance is administered. It accumulates in the lung and emits radiation. The radiation is recorded as a picture (scintigram) with a gamma camera.
Pulmonary embolism is one of the most frequent reasons for pulmonary scintigraphy. With this examination, even the smallest pulmonary embolism can be detected. If blood clots occlude pulmonary vessels, life-threatening embolisms occur.
Pulmonary scintigraphy may also be necessary prior to planned pulmonary operations (e.g., lung cancer) to estimate the postoperative remaining pulmonary function. This examination can also be used to calculate pathological changes in blood circulation, diseases of the cardio-pulmonary circulation or in congenital pulmonary malformations.

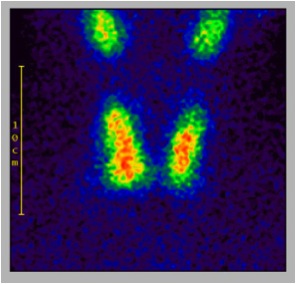
Figure: front view (RVL) and back view (LDR) from the lung – a pulmonary embolism is not existent and the blood supply is normal
Examination procedure
First, a small amount of a weakly radioactive substance is injected and shortly after it accumulates in the lungs.
The substances used are very well tolerated; allergic reactions are not known. The radiation load is low and quickly degraded.
Then images are recorded from the lung for approximately thirty minutes with a gamma camera.
The examination takes approximately one to two hours.
Preparation before and after the examination
A special preparation is not necessary. You do not need to be sober and can take your medication as usual.
We will send the examination results to your treating physician as soon as possible. The doctor will then contact you to discuss the results and any possible therapy.
If you have further questions, do not hesitate to contact us!
-
Kidney scintigraphy
Renal scintigraphy is a nuclear medical examination, which can be used to detect pathological changes in the kidneys. Thereto we will inject you a small amount of a low-radiation marker substance, which accumulates in the kidneys and emits radiation. According to the functional condition of the kidneys, the substance is excreted into the bladder via the ureters. This process is continuously tracked by a gamma camera in images (scintigrams).
The examination permits to draw conclusions about the blood flow, the function and urine flow of both kidneys and might be necessary in case of unexplained hypertension, in cases of urinary stasis (e.g., kidney stone), in congenital obstructive urinary flow disorders, in cases of tumours, impaired renal function, and after kidney transplantation.
Examination procedure
First, a small amount of a low-radiation marker substance is injected. After a while it accumulates in the kidneys.
The substances used are very well tolerated; allergic reactions are not known. The radiation load is low and quickly degraded.
A gamma camera records pictures of the kidney, which takes about thirty to forty-five minutes. During the examination, your blood will be collected and maybe you will get injected a diuretic.
The examination takes about an hour.
Preparation before and after the examination
Prior to the examination, please drink at least a half to one litre water.
You may have some meals before the examination.
If it is necessary to clarify a hypertension, you might need to discontinue some medication. If this is the case, we will discuss it with you or the referring physician.
We will send the examination results to your treating physician as soon as possible. He will then contact you to discuss the results as well as the possibility of a treatment.
Please do not hesitate to contact us if you any further questions!
-
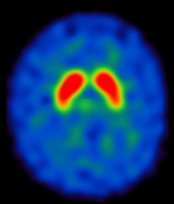
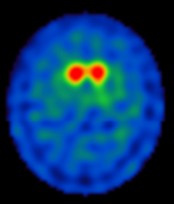
Brain scintigraphy
The scintigraphy of the dopamine transport density (DaTSCAN) is a nuclear medical examination in which the functionality of certain structures in the brain, so-called dopamine transporter, is examined. A low-radiation marker substance is administered and its distribution in the brain can then be tracked with a gamma camera and displayed as an image (scintigram).
The aim of the examination is to clarify an existing movement disorder. With DaTSCAN it is possible to visualize diseases such as Parkinson’s disease or Parkinson’s syndrome at a very early stage. They can be distinguished from harmless forms of “trembling” (Essential Tremor). The Essential Tremor is one of the most frequent movement disorders, which increases with age. Parkinsonian syndromes, on the other hand, are characterized by the fact that nerve cells are destroyed or altered in a certain area of the brain. These pathological modified cells can be detected with the DaTSCAN because the radiotracer accumulates there in a reduced form.

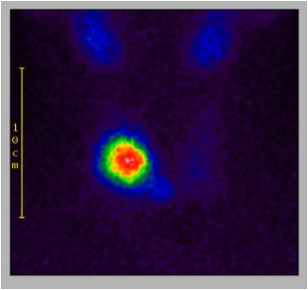
Figure left: normal findings.

Figure right: There is a reduced dopamine transporter density in the putamen which reveals the existence of Parkinson’s disease.
Examination procedure
First, you will get some drops of the drug Irenat® to protect the thyroid gland. Then a small amount of a low-radiation marker substance is injected, which accumulates in central brain regions (the striatum) within three to four hours.
The substances used are very well tolerated; allergic reactions are not known. The radiation load is low and quickly degraded.
After about three to four hours, we will take pictures of the brain with a gamma camera. You will lie on a stretcher as the camera rotates slowly around your head. These recordings will take approximately thirty minutes.
The entire examination will take about five to six hours. For the waiting period of three to four hours you do not have to stay at the practice. You may go home or go to work or to the DKD cafeteria.
Preparation before and after the examination
You may eat in advance to the examination.
You can take your medication as usual. However, we kindly ask you to bring a list of your medications with you.
Please drink a lot between injection of the substance and the images.
If a MRI has already been performed, please provide the images and the results beforehand.
The radiotracer is individually ordered for each patient and is not storable (the costs run several hundred euros). Hence we kindly ask you to always keep your appointment on time and if for any reason you need to reschedule or cancel your appointment please do this at least two days in advance.
We will send the examination results to your treating physician as soon as possible. He will then contact you to discuss the results as well as the possibility of a treatment.
Please do not hesitate to contact us if you have any further questions!
-
Parathyroid scintigraphy
The parathyroid scintigraphy is a nuclear medical examination with which possible malfunctions of the parathyroid gland (the so-called epithelium, which produce an important hormone for bone metabolism and calcium level) can be detected at a very early stage.
You will get a small amount of a low-radiation marker substance, which accumulates in the pathologically altered parathyroid gland and emits radiation. With a special gamma camera, the radiation can be visualized as image (scintigram).
With the examination, e.g. parathyroid gland nodes (adenomas) or hyperplasia can be detected and localized at a very early stage. This can facilitate the planning of surgical procedures. Adenoma is a benign neoplasm of glandular tissue. Hyperplasia is an increase of the glandular tissue, and consequently, an increased production of the Parathyroid hormone.
Examination procedure
First, a low-radiation marker substances radioactive substance is injected, which will accumulate after a while in the parathyroid glands.
The substances used are very well tolerated; allergic reactions are not known. The radiation load is low and quickly degraded.
After about half an hour we will take images with a gamma camera and repeat this procedure after one and after two hours.
The examination will take a total of about three hours and you may leave the practice during the waiting period.
Preparation before and after the examination
No special preparation is required and you can eat something in advance to the examination and can take your medication as usual.
We will send the examination results to your treating physician as soon as possible. He will then contact you to discuss the results as well as the possibility of a treatment.
Please do not hesitate to contact us if you have any further questions!
-
Sentinel lymph node scintigraphy
A scintigraphy of the sentinel lymph node (Sentinel Lymph Node) is a nuclear medical examination, which is used to detect the lymph node, which will be reached first by the lymphatic fluid of a malignant tumour. Hereto, a small amount of a low-radiation marker substance is administered and it accumulates in the lymphatic system on the way to the sentinel lymph node and emits radiation, which is subsequently recorded with a gamma camera as an image (scintigram). This allows to locate the sentinel lymph node.
Thousands of lymph nodes are connected by the lymphatic system. They form part of the body’s immune system. The lymph nodes are constructed like a filter which clears particles from the lymphatic fluid. Tumour cells can disseminate from a malignant tumour and be transported in the lymphatic system. The first lymph node reached by these cells stops them, enabling them to develop to a lymph node metastasis. This first lymph node is called the sentinel lymph node or “sentinel”. If this lymph node contains tumour cells it is very probable to find further metastases in the surrounding. However, if the sentinel lymph node is free from tumours, it is unlikely to find further metastases.
The scintigraphy of the sentinel node is especially used in breast cancer (breast carcinoma) and malignant melanoma. Prior to a tumour surgery, the sentinel lymph node is made visible and marked for removal. If it turns out that the sentinel lymph node contains no tumour cells, it can be assumed that all other lymph nodes are healthy/ free from tumour cells. By the targeted removal of the sentinel lymph node, most patients are spared from the removal of unaffected / healthy lymph nodes.
Examination procedure
The examination is usually done on the day of the surgery. First, a small amount of a low-radiation marker substance is injected into the area of the tumour. The substance is tracked her way through the lymphatic system to the sentinel lymph node by a gamma camera. This procedure takes a few minutes. The first lymph node reached by the substance (“the sentinel”) is marked on the patient’s skin.
The substances used are very well tolerated; allergic reactions are not known. The radiation load is low and quickly degraded.
A few hours later, the tumour and sentinel lymph nodes are removed surgically.
Preparation and time
No special preparation is required and you may have had something to eat during the day. You are also allowed to take your medication as usual.
The examination takes approximately one and a half hours.
Please do not hesitate to contact us, if you have any further questions!
-
Scintigraphy of the salivary glands
The scintigraphy of the salivary glands is a nuclear medical examination, with which the function of the salivary glands can be evaluated. Hereto, a low-radiation marker substance is administered. The substance accumulates in the salivary glands and emits radiation. A gamma camera records the radiation as image (scintigram).
With this examination, the function and secretion dysfunction of the four large salivary glands (parotid gland and submandibular gland) can be diagnosed, as well as inflammation or salivary stones. It is also performed to diagnose an oral dryness (e.g., Sjögren’s syndrom).
Examination procedure
First, we inject you a small amount of a low-radiation marker substance, which accumulates in the salivary glands after a few minutes.
The substances used are very well tolerated; allergic reactions are not known. The radiation load is low and quickly degraded.
Fifteen minutes later you will get some liquid, which you should swirl around in your mouth and then swallow. During injection and after receiving the liquid a gamma camera tracks images of the salivary glands.
The recording takes about twenty-five minutes.
Preparation before and after the examination
You should not eat one hour prior to the examination and only drink water.
Please do not take your medication for the salivary gland on the day of the examination. Other medication can be taken.
The examination takes about an hour.
We will send the examination results to your treating physician as soon as possible. He will then contact you to discuss the results as well as the possibility of a treatment.
Please do not hesitate to contact us if you have any further questions!
-
Others
Apart from the already described examinations, we also provide the following examinations:
Identification of the source of bleeding
Search of Inflammatory source (see also PET-CT and bone scintigraphy)
liver scintigraphy
Gastric emptying during scintigraphy
Adrenal glands scintigraphy
esophageal scintigraphy
Somatostatin receptor scintigraphy
Please do not hesitate to contact us if you need any further information!

 PET / CT (abbreviation for Positron Emission Tomography-Computed Tomography) is currently the most advanced imaging technique in cancer and dementia diagnostics. The combination of PET and CT in one device allows the detection of tumours, inflammations or neurological disorders earlier and more accurately than it was possible with previous methods.
PET / CT (abbreviation for Positron Emission Tomography-Computed Tomography) is currently the most advanced imaging technique in cancer and dementia diagnostics. The combination of PET and CT in one device allows the detection of tumours, inflammations or neurological disorders earlier and more accurately than it was possible with previous methods.